Introduction
The 2024 Medicare Physician Fee Schedule introduces new billing codes for caregiver training services, allowing eligible practitioners to bill Medicare for providing training and education to caregivers of patients with chronic illnesses or disabilities. This new provision aims to enhance patient care by equipping caregivers with the knowledge and skills needed to support their loved ones and manage their conditions effectively. It aligns with the 2022 National Strategy to Support Family Caregivers and the Biden-Harris Administration’s efforts to improve access to quality care and empower caregivers.
Background:
Each year since 1992, the Centers for Medicare and Medicaid Services (CMS) reviews payment practices under fee-for-service, or traditional, Medicare. The annually updated Medicare Physician Fee Schedule (PFS) also outlines significant policy changes for Medicare part B. The most recent Medicare PFS was finalized in early November and is effective January 1, 2024, and it includes a number of changes aimed at improving services available for family caregivers and the Medicare beneficiaries under their care.
Most notably, the CY 2024 Medicare Physician Fee Schedule includes payments for physicians and other clinical practitioners to provide education and training to family caregivers. The final rule also includes new payments proposed for services that address health-related social needs (HRSNs) and improve access to mental and behavioral health treatment. These additions represent consequential advancement toward achieving core policy principles and proposals outlined in various administration initiatives to improve support for family caregivers. These important federal frameworks include, but are not limited to:
- Executive Order on Increasing Access to High-Quality Care and Supporting Caregivers
- 2022 National Strategy to Support Family Caregivers
- Cancer Moonshot
- Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government
- HHS’s Strategic Approach to Addressing Social Determinants of Health to Advance Health Equity
In September, the National Alliance for Caregiving (NAC) submitted comments to CMS in response to their draft changes. Overall, NAC’s comments commended CMS for including proposals in the CY 2024 Medicare PFS aligned with the Goal 2[1]of the 2022 National Strategy to Support Family Caregivers to leverage existing federal agency authority to 1) boost the supply of education and long-term care and to provide support for family caregivers; 2) support family caregivers of beneficiaries of federal health care programs and services; 3) recognize and address systemic barriers to healthcare services and benefits for people of color and other underserved groups; and 4) help patients, families, and caregivers better navigate the caregiving experience.
ABOUT THE NATIONAL STRATEGY TO SUPPORT FAMILY CAREGIVERS
The 2022 National Strategy to Support Family Caregivers is the first whole-of-society blueprint to support family caregivers of all ages, from youth to grandparents, and regardless of where they live or what caregiving looks like for them and their loved ones.
The strategy includes nearly 350 actions that federal agencies will take in the next 3 years, as well as specific actions that states, communities, health care systems, long-term support and service providers, researchers, employers, philanthropic organizations, and many others can take to make these goals a reality.
Goals of the National Strategy
- Increase awareness of, and outreach to, family caregivers
- Advance inclusion and engagement of family caregivers within care teams
- Advance innovations in family caregiver services and supports
- Strengthen financial and workplace security of family caregivers
- Advance a family caregiver national research and data collection strategy
The Role of Family Caregivers in Healthcare
Caregivers are essential participants in a patient’s care team but have historically been unrecognized and unsupported. According to recent research conducted by NAC and AARP[1], nearly six in 10 family caregivers assist with medical and nursing tasks such as injections, tube feedings and changing catheters. Unfortunately, according to the same report, fewer than three in 10 caregivers surveyed (29 percent) said they have had general conversations with health professionals, such as a doctor, nurse, or social worker, about their caregiving duties. Only 13 percent said a health care professional has asked what they need to take care of themselves.
Furthermore, only seven percent report receiving any training related to tasks they perform[1]. Black and Latino American caregivers (67 percent each) more often help with medical/nursing tasks than do White caregivers (52 percent). While four in 10 caregivers are in high-intensity caregiving situations (40 percent) the proportion of caregivers (31 percent) who reported difficulty in coordinating care among health care providers is growing[2].
Demographics portend that absent significant and cross-cutting action from federal policy makers, these challenges will become more acute. The population of older adults—the majority of Medicare beneficiaries needing care—is growing at an historic rate, necessitating the support of increasing numbers of family caregivers. In fact, between 2015 and 2020, the number of unpaid family caregivers increased by more than 10 million, to 53 million family caregivers according to research from NAC and AARP. However, the ratio of available caregivers to those who need care is declining. Existing national programs to support caregivers are vital but insufficiently funded to meet the need. CMS leadership and engagement is crucial to national efforts aimed at shifting the trajectory of these statics.
The CY 2024 Physician Fee Schedule recognizes that family caregivers are essential participants in a patient’s care team
The Department of Health and Human Services (HHS) and CMS serve a critical role in ensuring that the federal government achieves the ambitious, but essential, goals outlined to support family caregivers in the National Strategy–a population that has been historically underrepresented and underserved in federal health care policy deliberations and decisions. By bolstering access to training and support services for caregivers, the CY 2024 Medicare PFS makes progress toward addressing the demographic challenges inherent in a growing older adult population but declining number of available and willing family caregivers. This is a critical step in recognizing the essential role that family caregivers play in safeguarding the health of American families[3].
Caregiver Training Services
Specifically, the CY 2024 Medicare PFS includes specific CPT payment codes for individual and group caregiver training services (CTS) for patients with a mental or physical health diagnosis as well as caregivers for patients who need help with activities of daily living (ADLs) and instrumental ADLs. While payment for CTS was recommended by the American Medical Association (AMA) and NAC several years ago, CMS traditionally does not pay practitioners under Medicare Part B to deliver services to individuals other than the patient–especially when the patient is not present. CMS recognizes the “extensive empirical support” that appropriate and adequate training for caregivers as part of a person-centered care plan promotes improved patient outcomes. Subsequently, the CY 2024 Medicare PFS includes payment for CTS starting on January 1.
CPT Codes in Detail
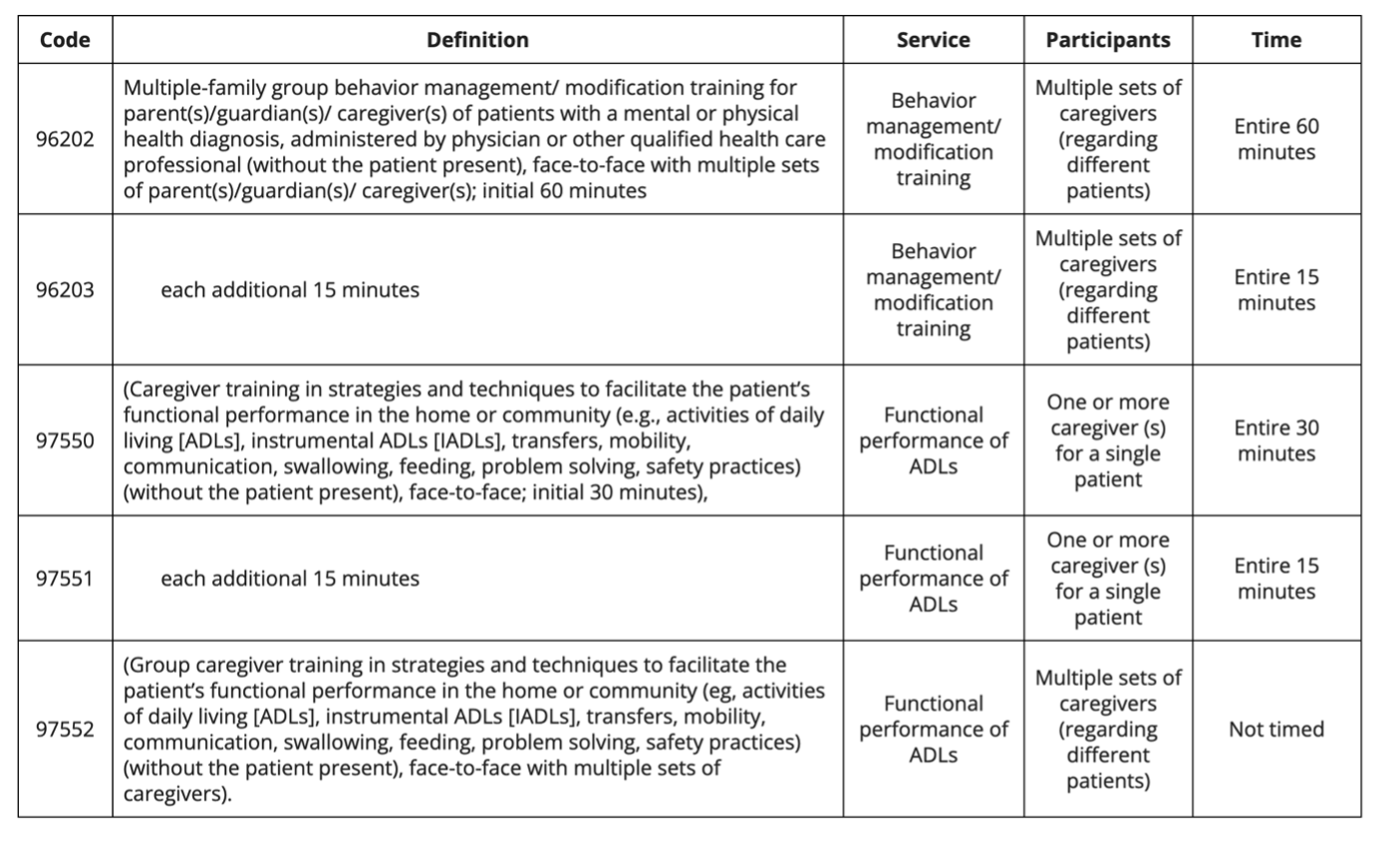
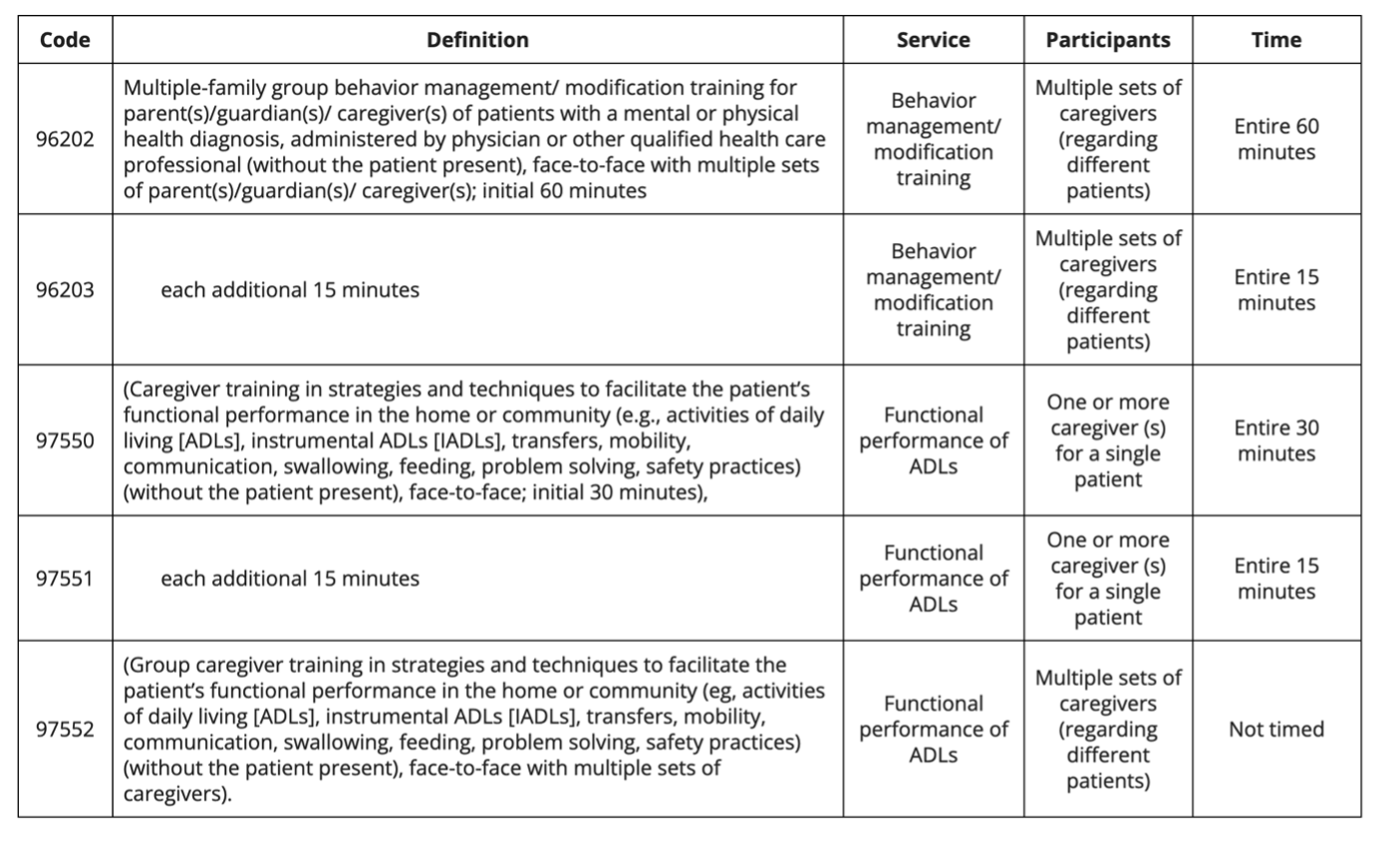
CMS will recognize and pay for two existing CPT® codes, which in 2023 had a status indicator of bundled (96202 and 96203), and three new CPT® codes that will allow physicians and other qualified health care professionals to provide training for caregivers of patients (97550-97552)
One set of codes (96202, 96203) is for group training in behavior management/modification of patients with a mental or physical health diagnosis. The group training would include caregivers of different patients.
Two of the new codes, 97550 and 97551 are for caregivers of an individual patient to facilitate the patient’s functional performance in their home and community relating to Activities of Daily Living. (ADL) These are timed codes, 30 minutes and 15 minutes respectively. The third new code, 97552 is for group training of multiple sets of caregivers (who are caring for different patients). That group training code is not assigned a time.
Provider Coverage
Effective January 1, 2024, Medicare practitioners (including physicians, nonphysician practitioners (NPPs), or physical, occupational, or speech therapists) can bill for engagement and training with patient caregivers as training relates to a patient’s treatment plan.
CMS Definition of Caregiver
NAC encouraged CMS to expand the originally included definition of caregiver to better reflect existing federal programs and policies addressing caregivers and the caregiver/patient experience. Specifically, NAC encouraged CMS to consider aligning the definition of caregiver with existing statutes and administration priorities that define caregivers. For example, the Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act (P.L. 115-119) defines the term “family caregiver” as “an adult family member or other individual who has a significant relationship with, and who provides a broad range of assistance to, an individual with a chronic or other health condition, disability, or functional limitation.”
In response, CMS updated the CY 2024 Medicare PFS definition of caregiver to reflect the RAISE Act noting that the Act influenced the initial CTS proposals. As revised, a caregiver is defined in the final rule as, “an adult family member or other individual who has a significant relationship with, and who provides a broad range of assistance to, an individual with a chronic or other health condition, disability, or functional limitation’’ and ‘‘a family member, friend, or neighbor who provides unpaid assistance to a person with a chronic illness or disabling condition’’.
Sessions Covered
Additionally, the final CY 2024 Medicare PFS aligns with NAC comments that permit practitioners to provide more than one session of CTS delivery per year. CMS acknowledged comments from myriad advocates noting that the needs of patients with complex illness evolve over time as their conditions change and/or they are diagnosed with additional illnesses. Furthermore, CMS recognized that there may be more than one person caring for an individual beneficiary and/or that one caregiver may be providing support for multiple beneficiaries. As such, CMS finalized the proposal to provide “reasonable and necessary” CTS determined by the practitioner and according to the “volume and frequency” required by the patient’s care plan.
CTS Services: Not a Substitute for Other Benefits
CMS also outlined that “CTS services have their place in a reasonable and necessary treatment plan for some patients and can serve as an important supplement to other caregiver training and other resources that might be available.” These and other provisions in the final rule align with NAC’s comments that CTS are not duplicative of other federally funded caregiver support programs, and that they should be provided supplemental to–rather than as a substitute for–any additional benefits for which patients are eligible.Opportunities for Future Updates to CTS
While CMS rejected some recommendations from NAC and other commenters related to CTS, the final rule notes that the agency will continue to consider whether these recommendations should be incorporated in future rulemaking. For example, the CY 2024 Medicare PFS does not permit alternative methods of CTS delivery–including via telehealth–nor does it permit additional auxiliary personnel operating under general supervision of the Medicare provider or NPP to provide CTS. Furthermore, CMS acknowledged the importance of–but declined to include–standards or quality requirements for CTS activities. The agency also determined that physical and behavioral health examples included in the proposed rule sufficiently represented the types of conditions that could necessitate CTS, and did not expand the referenced circumstances. However, advocates should continue to communicate these and other needed policy updates as CTS services are implemented in 2024 and beyond.
Consent and Co-Payment Required for CTS
The National Alliance for Caregiving did not comment about the proposed consent or co-payment requirements for CTS, but it is important to note that the final rule requires patient consent to deliver caregiver training services because those services will be delivered without the patient present. The final rule specifically states that providers will need to obtain consent for CTS directly, and that CTS will not be covered under a patient’s general consent to receive treatment.
Furthermore, CMS states consent is necessary because any applicable cost-sharing requirements will be the patient’s responsibility. Because CTS will be a Medicare Part B service, deductible and coinsurance requirements will apply. While Medicaid and Medigap coverage may cover some or all of these costs for eligible and enrolled beneficiaries, the provider cannot elect to waive the deductible or cost-sharing requirement for CTS.
Additional provisions in the CY 2024 Medicare PFS that Will Affect Family Caregivers
In the final rule, CMS implemented the proposed expansive steps to recognize the distinct impact that Health-Related Social Needs (HRSNs) contributes to negative health outcomes and increased total cost of care for beneficiaries. Specifically, the agency finalized new billing codes for Community Health Integration (CHI), Social Determinants of Health (SDOH) Risk Assessment, and Principal Illness Navigation (PIN) services delivered by health care support staff, including community health workers, care navigators, and peer support specialists.
These services are meant to address unmet SDOH needs that will affect the diagnosis or treatment of a patient and to help Medicare beneficiaries with high-risk conditions, such as dementia or cancer, connect with clinical and supportive services resources. These are an important and forward-looking approach to support a whole-person model of care, which can reduce the immense burden that family caregivers face.
Furthermore, CMS finalized proposals aimed at improving support for emotional and mental well-being through their behavioral health care. These changes to improve access to behavioral health will allow clinical social workers, marriage and family therapists, and mental health counselors, including addiction counselors, to enroll in Medicare and bill for their services. Given that an estimated 13 million caregivers support adults with mental health conditions and substance use conditions,[1] expanded access to health behavior assessment and intervention (HBAI) services is a critical component to supporting caregivers.
Conclusion
Overall, the changes and additions included in the CY 2024 Medicare Physician Fee Schedule represent a broader whole-of-government approach to improve supports for family caregivers, reflect the input and wisdom of caregiver advocates, and are a milestone toward achieving Goal 2 of the National Strategy and to building a society that values, supports, and empowers America’s 53 million family caregivers.
Table of Contents
- Introduction
- Background
- The Role of Family Caregivers in Healthcare
- The CY 2024 Physician Fee Schedule recognizes that family caregivers are essential participants in a patient’s care team
- Caregiver Training Services
- CPT Codes in Detail
- Provider Coverage
- CMS Definition of Caregiver
- Sessions Covered
- CTS Services: Not a Substitute for Other Benefits
- Consent and Co-Payment Required for CTS
- Additional provisions in the CY 2024 Medicare PFS that Will Affect Family Caregivers
- Conclusion
Table of Contents
- Introduction
- Background
- The Role of Family Caregivers in Healthcare
- The CY 2024 Physician Fee Schedule recognizes that family caregivers are essential participants in a patient’s care team
- Caregiver Training Services
- CPT Codes in Detail
- Provider Coverage
- CMS Definition of Caregiver
- Sessions Covered
- CTS Services: Not a Substitute for Other Benefits
- Consent and Co-Payment Required for CTS
- Additional provisions in the CY 2024 Medicare PFS that Will Affect Family Caregivers
- Conclusion
Introduction
The 2024 Medicare Physician Fee Schedule introduces new billing codes for caregiver training services, allowing eligible practitioners to bill Medicare for providing training and education to caregivers of patients with chronic illnesses or disabilities. This new provision aims to enhance patient care by equipping caregivers with the knowledge and skills needed to support their loved ones and manage their conditions effectively. It aligns with the 2022 National Strategy to Support Family Caregivers and the Biden-Harris Administration’s efforts to improve access to quality care and empower caregivers.
Background:
Each year since 1992, the Centers for Medicare and Medicaid Services (CMS) reviews payment practices under fee-for-service, or traditional, Medicare. The annually updated Medicare Physician Fee Schedule (PFS) also outlines significant policy changes for Medicare part B. The most recent Medicare PFS was finalized in early November and is effective January 1, 2024, and it includes a number of changes aimed at improving services available for family caregivers and the Medicare beneficiaries under their care.
Most notably, the CY 2024 Medicare Physician Fee Schedule includes payments for physicians and other clinical practitioners to provide education and training to family caregivers. The final rule also includes new payments proposed for services that address health-related social needs (HRSNs) and improve access to mental and behavioral health treatment. These additions represent consequential advancement toward achieving core policy principles and proposals outlined in various administration initiatives to improve support for family caregivers. These important federal frameworks include, but are not limited to:
- Executive Order on Increasing Access to High-Quality Care and Supporting Caregivers
- 2022 National Strategy to Support Family Caregivers
- Cancer Moonshot
- Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government
- HHS’s Strategic Approach to Addressing Social Determinants of Health to Advance Health Equity
In September, the National Alliance for Caregiving (NAC) submitted comments to CMS in response to their draft changes. Overall, NAC’s comments commended CMS for including proposals in the CY 2024 Medicare PFS aligned with the Goal 2[1]of the 2022 National Strategy to Support Family Caregivers to leverage existing federal agency authority to 1) boost the supply of education and long-term care and to provide support for family caregivers; 2) support family caregivers of beneficiaries of federal health care programs and services; 3) recognize and address systemic barriers to healthcare services and benefits for people of color and other underserved groups; and 4) help patients, families, and caregivers better navigate the caregiving experience.
ABOUT THE NATIONAL STRATEGY TO SUPPORT FAMILY CAREGIVERS
The 2022 National Strategy to Support Family Caregivers is the first whole-of-society blueprint to support family caregivers of all ages, from youth to grandparents, and regardless of where they live or what caregiving looks like for them and their loved ones.
The strategy includes nearly 350 actions that federal agencies will take in the next 3 years, as well as specific actions that states, communities, health care systems, long-term support and service providers, researchers, employers, philanthropic organizations, and many others can take to make these goals a reality.
Goals of the National Strategy
- Increase awareness of, and outreach to, family caregivers
- Advance inclusion and engagement of family caregivers within care teams
- Advance innovations in family caregiver services and supports
- Strengthen financial and workplace security of family caregivers
- Advance a family caregiver national research and data collection strategy
The Role of Family Caregivers in Healthcare
Caregivers are essential participants in a patient’s care team but have historically been unrecognized and unsupported. According to recent research conducted by NAC and AARP[1], nearly six in 10 family caregivers assist with medical and nursing tasks such as injections, tube feedings and changing catheters. Unfortunately, according to the same report, fewer than three in 10 caregivers surveyed (29 percent) said they have had general conversations with health professionals, such as a doctor, nurse, or social worker, about their caregiving duties. Only 13 percent said a health care professional has asked what they need to take care of themselves.
Furthermore, only seven percent report receiving any training related to tasks they perform[1]. Black and Latino American caregivers (67 percent each) more often help with medical/nursing tasks than do White caregivers (52 percent). While four in 10 caregivers are in high-intensity caregiving situations (40 percent) the proportion of caregivers (31 percent) who reported difficulty in coordinating care among health care providers is growing[2].
Demographics portend that absent significant and cross-cutting action from federal policy makers, these challenges will become more acute. The population of older adults—the majority of Medicare beneficiaries needing care—is growing at an historic rate, necessitating the support of increasing numbers of family caregivers. In fact, between 2015 and 2020, the number of unpaid family caregivers increased by more than 10 million, to 53 million family caregivers according to research from NAC and AARP. However, the ratio of available caregivers to those who need care is declining. Existing national programs to support caregivers are vital but insufficiently funded to meet the need. CMS leadership and engagement is crucial to national efforts aimed at shifting the trajectory of these statics.
The CY 2024 Physician Fee Schedule recognizes that family caregivers are essential participants in a patient’s care team
The Department of Health and Human Services (HHS) and CMS serve a critical role in ensuring that the federal government achieves the ambitious, but essential, goals outlined to support family caregivers in the National Strategy–a population that has been historically underrepresented and underserved in federal health care policy deliberations and decisions. By bolstering access to training and support services for caregivers, the CY 2024 Medicare PFS makes progress toward addressing the demographic challenges inherent in a growing older adult population but declining number of available and willing family caregivers. This is a critical step in recognizing the essential role that family caregivers play in safeguarding the health of American families[3].
Caregiver Training Services
Specifically, the CY 2024 Medicare PFS includes specific CPT payment codes for individual and group caregiver training services (CTS) for patients with a mental or physical health diagnosis as well as caregivers for patients who need help with activities of daily living (ADLs) and instrumental ADLs. While payment for CTS was recommended by the American Medical Association (AMA) and NAC several years ago, CMS traditionally does not pay practitioners under Medicare Part B to deliver services to individuals other than the patient–especially when the patient is not present. CMS recognizes the “extensive empirical support” that appropriate and adequate training for caregivers as part of a person-centered care plan promotes improved patient outcomes. Subsequently, the CY 2024 Medicare PFS includes payment for CTS starting on January 1.
CPT Codes in Detail
CMS will recognize and pay for two existing CPT® codes, which in 2023 had a status indicator of bundled (96202 and 96203), and three new CPT® codes that will allow physicians and other qualified health care professionals to provide training for caregivers of patients (97550-97552)
One set of codes (96202, 96203) is for group training in behavior management/modification of patients with a mental or physical health diagnosis. The group training would include caregivers of different patients.
Two of the new codes, 97550 and 97551 are for caregivers of an individual patient to facilitate the patient’s functional performance in their home and community relating to Activities of Daily Living. (ADL) These are timed codes, 30 minutes and 15 minutes respectively. The third new code, 97552 is for group training of multiple sets of caregivers (who are caring for different patients). That group training code is not assigned a time.
Provider Coverage
Effective January 1, 2024, Medicare practitioners (including physicians, nonphysician practitioners (NPPs), or physical, occupational, or speech therapists) can bill for engagement and training with patient caregivers as training relates to a patient’s treatment plan.
CMS Definition of Caregiver
NAC encouraged CMS to expand the originally included definition of caregiver to better reflect existing federal programs and policies addressing caregivers and the caregiver/patient experience. Specifically, NAC encouraged CMS to consider aligning the definition of caregiver with existing statutes and administration priorities that define caregivers. For example, the Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act (P.L. 115-119) defines the term “family caregiver” as “an adult family member or other individual who has a significant relationship with, and who provides a broad range of assistance to, an individual with a chronic or other health condition, disability, or functional limitation.”
In response, CMS updated the CY 2024 Medicare PFS definition of caregiver to reflect the RAISE Act noting that the Act influenced the initial CTS proposals. As revised, a caregiver is defined in the final rule as, “an adult family member or other individual who has a significant relationship with, and who provides a broad range of assistance to, an individual with a chronic or other health condition, disability, or functional limitation’’ and ‘‘a family member, friend, or neighbor who provides unpaid assistance to a person with a chronic illness or disabling condition’’.
Sessions Covered
Additionally, the final CY 2024 Medicare PFS aligns with NAC comments that permit practitioners to provide more than one session of CTS delivery per year. CMS acknowledged comments from myriad advocates noting that the needs of patients with complex illness evolve over time as their conditions change and/or they are diagnosed with additional illnesses. Furthermore, CMS recognized that there may be more than one person caring for an individual beneficiary and/or that one caregiver may be providing support for multiple beneficiaries. As such, CMS finalized the proposal to provide “reasonable and necessary” CTS determined by the practitioner and according to the “volume and frequency” required by the patient’s care plan.
CTS Services: Not a Substitute for Other Benefits
CMS also outlined that “CTS services have their place in a reasonable and necessary treatment plan for some patients and can serve as an important supplement to other caregiver training and other resources that might be available.” These and other provisions in the final rule align with NAC’s comments that CTS are not duplicative of other federally funded caregiver support programs, and that they should be provided supplemental to–rather than as a substitute for–any additional benefits for which patients are eligible.Opportunities for Future Updates to CTS
While CMS rejected some recommendations from NAC and other commenters related to CTS, the final rule notes that the agency will continue to consider whether these recommendations should be incorporated in future rulemaking. For example, the CY 2024 Medicare PFS does not permit alternative methods of CTS delivery–including via telehealth–nor does it permit additional auxiliary personnel operating under general supervision of the Medicare provider or NPP to provide CTS. Furthermore, CMS acknowledged the importance of–but declined to include–standards or quality requirements for CTS activities. The agency also determined that physical and behavioral health examples included in the proposed rule sufficiently represented the types of conditions that could necessitate CTS, and did not expand the referenced circumstances. However, advocates should continue to communicate these and other needed policy updates as CTS services are implemented in 2024 and beyond.
Consent and Co-Payment Required for CTS
The National Alliance for Caregiving did not comment about the proposed consent or co-payment requirements for CTS, but it is important to note that the final rule requires patient consent to deliver caregiver training services because those services will be delivered without the patient present. The final rule specifically states that providers will need to obtain consent for CTS directly, and that CTS will not be covered under a patient’s general consent to receive treatment.
Furthermore, CMS states consent is necessary because any applicable cost-sharing requirements will be the patient’s responsibility. Because CTS will be a Medicare Part B service, deductible and coinsurance requirements will apply. While Medicaid and Medigap coverage may cover some or all of these costs for eligible and enrolled beneficiaries, the provider cannot elect to waive the deductible or cost-sharing requirement for CTS.
Additional provisions in the CY 2024 Medicare PFS that Will Affect Family Caregivers
In the final rule, CMS implemented the proposed expansive steps to recognize the distinct impact that Health-Related Social Needs (HRSNs) contributes to negative health outcomes and increased total cost of care for beneficiaries. Specifically, the agency finalized new billing codes for Community Health Integration (CHI), Social Determinants of Health (SDOH) Risk Assessment, and Principal Illness Navigation (PIN) services delivered by health care support staff, including community health workers, care navigators, and peer support specialists.
These services are meant to address unmet SDOH needs that will affect the diagnosis or treatment of a patient and to help Medicare beneficiaries with high-risk conditions, such as dementia or cancer, connect with clinical and supportive services resources. These are an important and forward-looking approach to support a whole-person model of care, which can reduce the immense burden that family caregivers face.
Furthermore, CMS finalized proposals aimed at improving support for emotional and mental well-being through their behavioral health care. These changes to improve access to behavioral health will allow clinical social workers, marriage and family therapists, and mental health counselors, including addiction counselors, to enroll in Medicare and bill for their services. Given that an estimated 13 million caregivers support adults with mental health conditions and substance use conditions,[1] expanded access to health behavior assessment and intervention (HBAI) services is a critical component to supporting caregivers.
Conclusion
Overall, the changes and additions included in the CY 2024 Medicare Physician Fee Schedule represent a broader whole-of-government approach to improve supports for family caregivers, reflect the input and wisdom of caregiver advocates, and are a milestone toward achieving Goal 2 of the National Strategy and to building a society that values, supports, and empowers America’s 53 million family caregivers.

